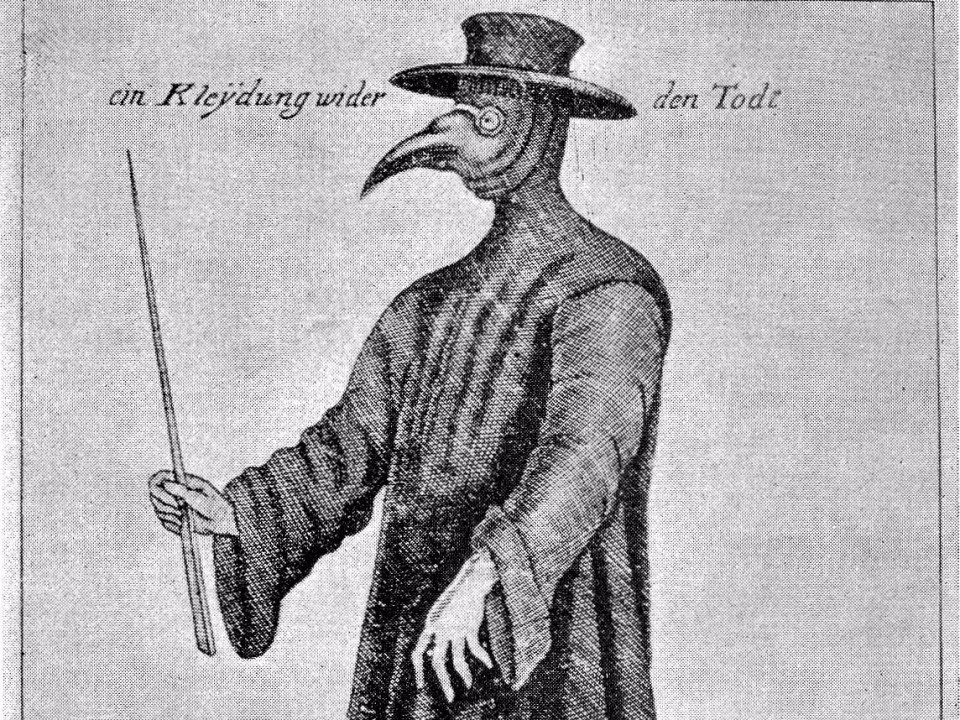
If you told me I’d be working out of the home office and we’d be in the middle of a global pandemic, like many of us, or maybe all of us, I’d scoff at the idea. I’d Google “pandemic” and become completely engrossed with those Black-Death bird masks of the bubonic plague era, and wonder how many of them I’d see at Halloween parties this year.
Unfortunately, this has become a reality and as with any “change in plans” so to speak, after accepting the situation, I’m becoming more and more enthusiastic about us coming out the other end as more intelligent, flexible people and organizations. I’m also realizing that there may not be Halloween parties at all this year. At least not in person.
At Streamline Healthcare Solutions, we see the lock-down as transformational for the health and human services market. I reached out to CEO’s and clinical directors as they were transitioning to telehealth and phone-based therapy. Fortunately, regulatory requirements from the federal government and payers have been adapted and providers are being reimbursed for both telehealth and phone-based visits, and at a higher rate. As with many transformations, we’ve been forced to change because of desperation, not virtue, but I think we will come out the other side more flexible and resilient.
The current technology we are using is not new. It’s really about utilizing the technology we have today to adapt to the current environment and come out stronger. Any type of evolution in my life came with a healthy dose of pain. Pain brings a new openness to other possibilities. As we all adapt to the new normal, opportunities will be provided to those organizations that embrace this change and push it further.
I’ve been working in the health and human services technology field for twenty years now. Prior to that, I worked in residential traumatic brain injury rehab services through college totaling about ten years.
Medicaid is state run, so every state has a slightly different process for reimbursing these services. The best hope as of today is slowly moving the needle and standardizing the processes within each state first, and then hopefully on the national level. On average, Medicaid reimburses 70% of the commercial rates paired with a high administrative burden with differing requirements per state. Providing flexible work at home policies, and/or shared work spaces lowers organizational costs and retains staff. Future investments will be on training and technology, not on office space.
If someone is on Medicaid, they are most likely going through a very rough time to begin with, and most mental health issues are chronic conditions.
Not all clients, but a good percentage of our clients will appreciate the flexibility of connecting via telehealth meetings with their primary therapist, clinical team, or peer supports. Here are a couple of areas where the “virtual” will become the standard process in the health and human services market.
1. Payers will provide clear guidelines and payment structures for telehealth and phone-based services. Teams can connect with clients on a more regular basis increasing data points for continual progress.
2. National clinical licensure will become the norm promoting specific individual clinical expertise over state regulatory agencies.
3. Telehealth training and certification will become a “thing”. Clinical staff will be formally trained and certified to provide services remotely and depending on the client, specific timeframes for face-to-face meetings.
4. Telehealth training will become a process that both clients and family members will go through. Clients will be coached on building a private, secure at-home environment to speak openly with their therapist.
5. A majority of intake processes will become completely virtual. Clients who call in will be immediately provided access to a patient portal for both the gathering and double-checking health information. Same-day initial intake meetings will take place and immediate access to same-day virtual clinical assessment will take place, hopefully lowering higher levels of care access.
6. Clinical teams will meet with clients, families, case managers, and insurance companies virtually. No clinical reviews or meetings will be done in-person unless necessary. The clinical information can be shared easily via video conferencing bringing both paper charts and CCD’s to life.
7. Data Use. In the simplest terms, what we call “Alerts” today will become a reordering of focus on the client. Rather than be “alerted” to a past due medication refill, clinicians will be alerted on the possible outcomes based on clinical data. Clinical teams will be able to look at their clients against state and national populations with the same diagnosis and disease.
8. Client Portals will be utilized by clients on a daily basis. As the communication becomes more virtual, clinical staff will require more written feedback and data points on a client’s progress.
9. Group Sessions. As we’ve seen with a number of groups like Alcoholics Anonymous, therapeutic groups have moved on-line quickly. With the right process, the ability to share and provide feedback will become an option for some groups.
10. Incorporation of client-facing applications that add to the clinical process and do not “crowd out” daily living. Clients can use applications for education and reminders for medications and track vitals.
As organizations future evaluate and define the clients and staff that can succeed and strive in the virtual environment, we will see the streamlining and financial savings for these types of services. Just like we’ve never gone back to writing letters and moved to email, the virtual therapy session is here to stay. The next step in this process is seeing how we can make it work for the largest amounts, or particular types of clients and how we can improve quality through the usage of this technology. Organizations will take this opportunity to focus on connections and outcomes rather than seeing their clients face-to-face.