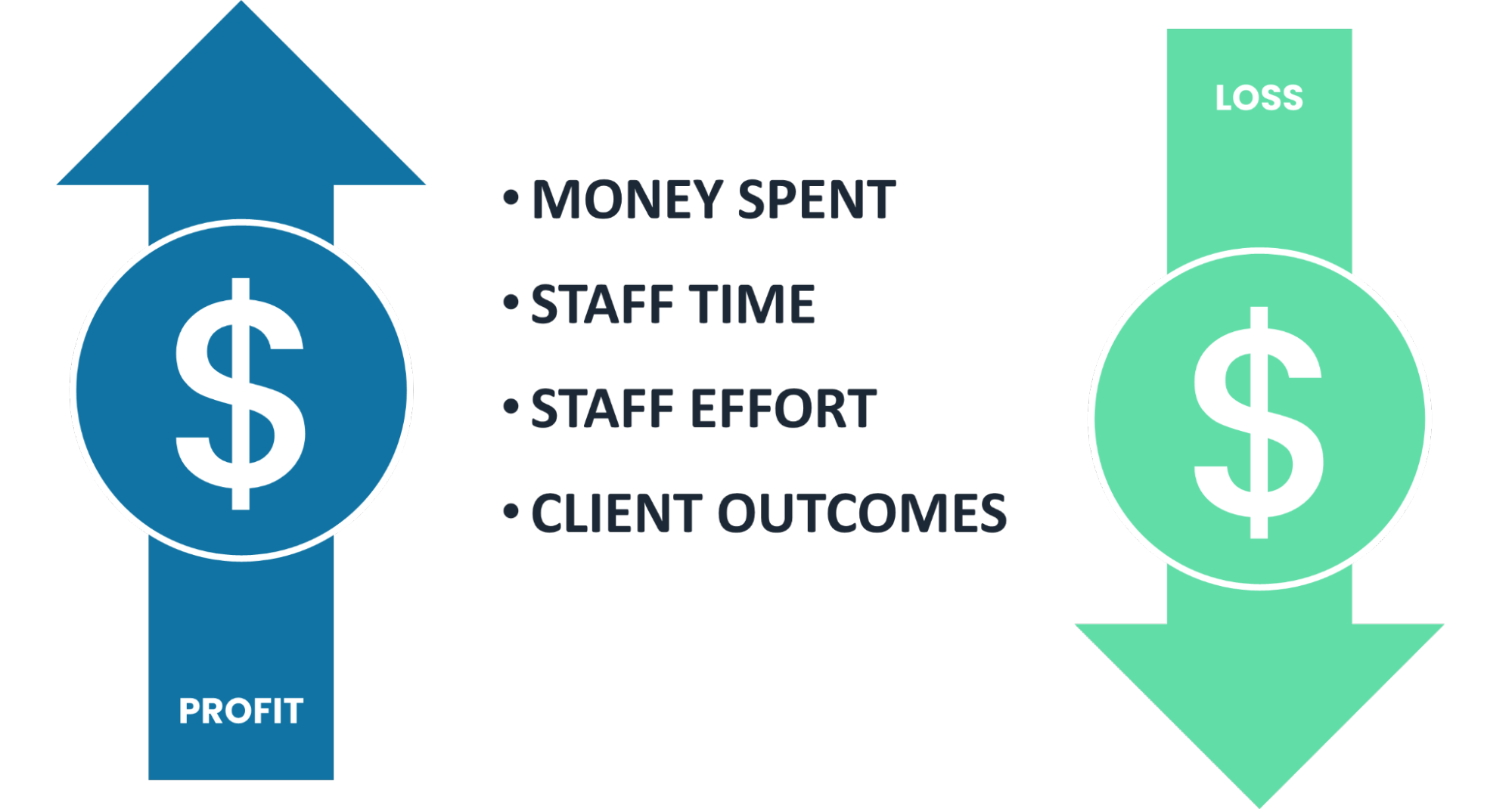
For substance abuse and mental health treatment providers, a new Electronic Health Record (EHR) system is a big commitment. Implementing it requires significant investments of both time and money, with a lot of pressure to get it right.
Your EHR is critical to your organization’s success. How you use your EHR is equally crucial as which EHR. The electronic health record will be the backbone of your organization. It can provide insightful information regarding your organization and patient outcomes if used correctly.
Standard productivity tools like Microsoft Word and Excel have expanded our capabilities and dramatically lowered the friction of presenting and sharing information. But like many technologies, you usually use around 20 percent of the available features. That may seem “good enough” to get the job done. However, learning to take advantage of more features and functionality can get you better results and a better return on investment (ROI).
How can you launch your new EHR in a way that gets the most ROI? Here are some critical steps in the EHR implementation process.
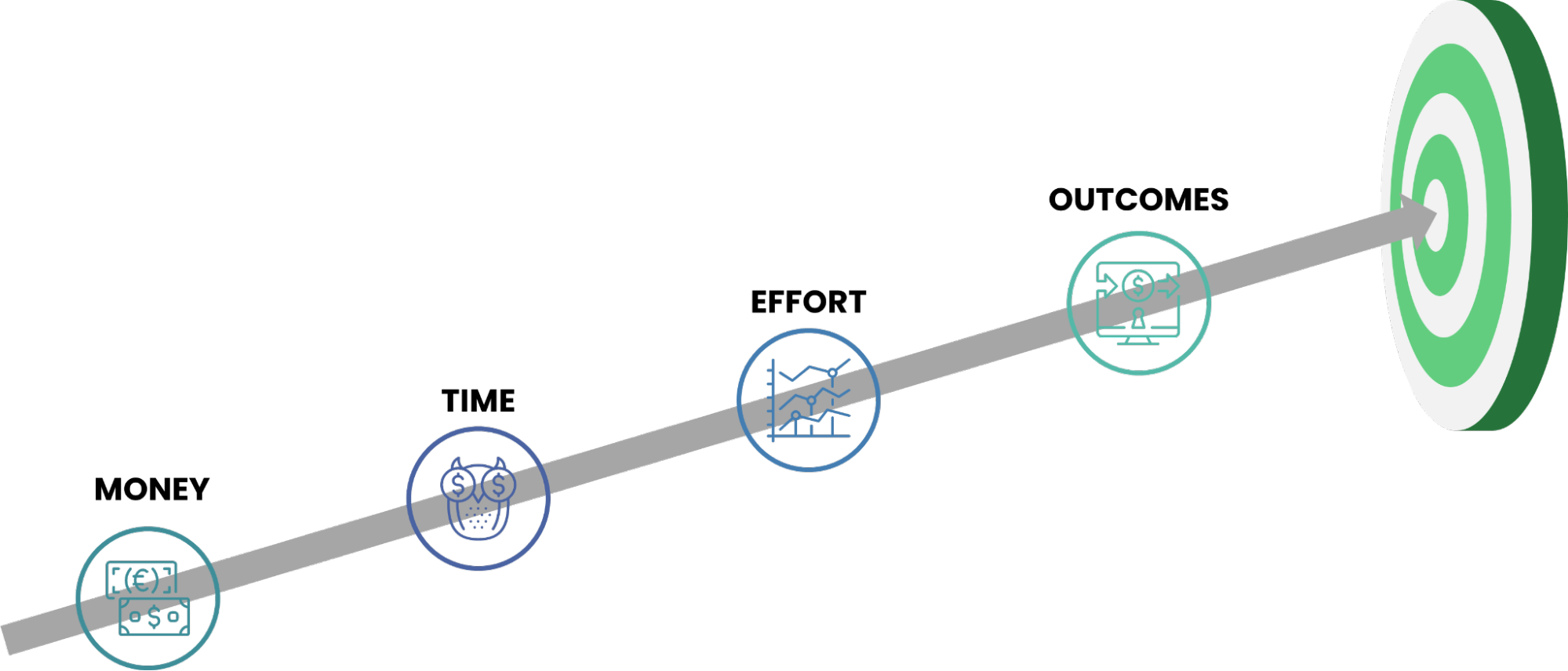
Measure where you are today and set your future goals
At the start of any technology implementation, you should be thoroughly familiar with your organization, levels of care, processes, and protocols.
You should also understand how existing processes, technology, and staff work together. Be sure to plan and visualize what you want the organization to look like, where you want it to go, and your goals. How do you measure against your peers or national averages? How do you measure success internally? Consider how you will continue using the new EHR years later. Make sure you have the staff you need to make it all work.
Next, determine how you will measure your goals and whether you have succeeded. How will the EHR help you accomplish those goals, and how will you make it a complete success? How will you measure that success? These are the answers you need before proceeding.
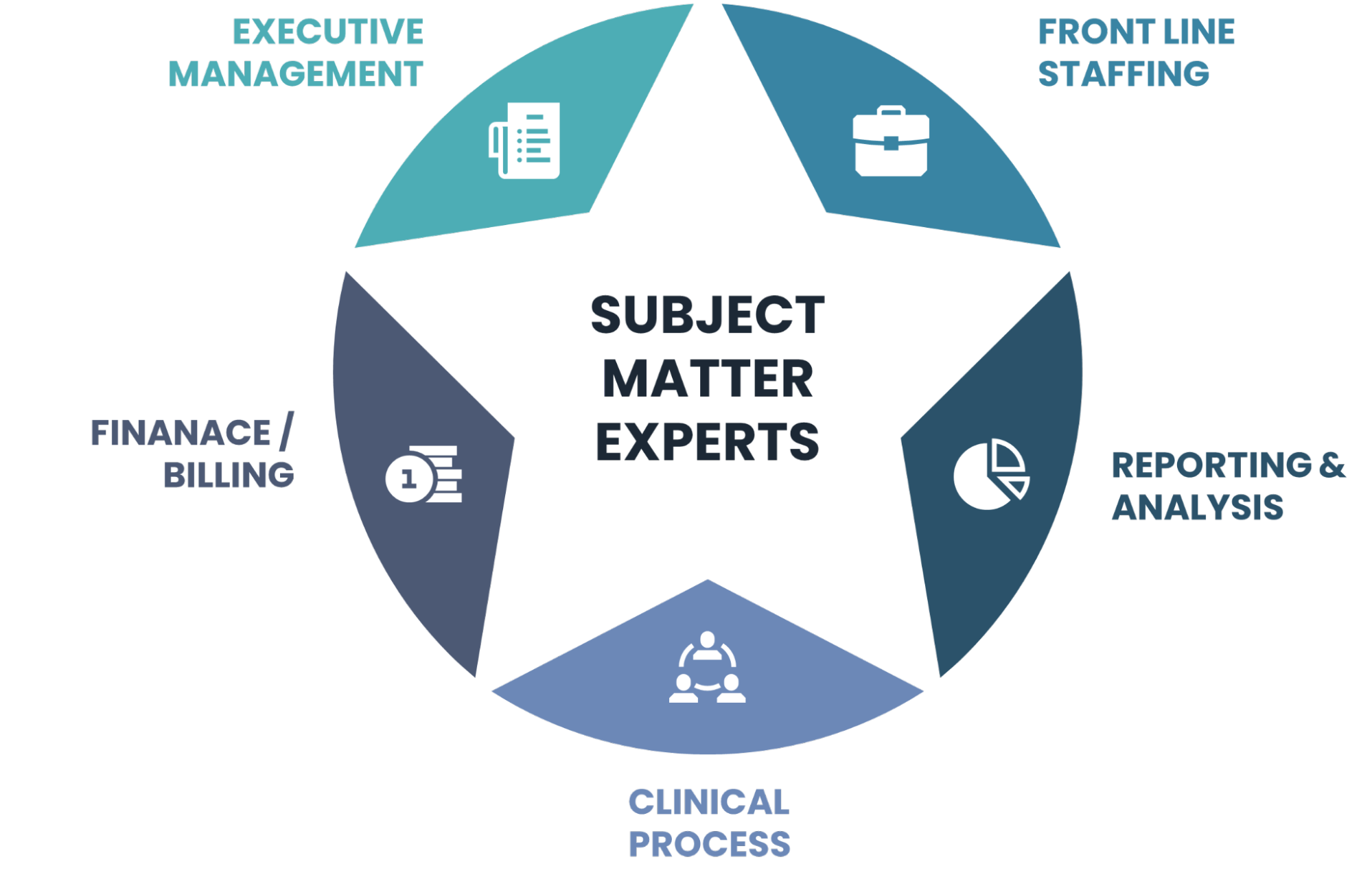
Create an implementation team
Your practice or organization should organize a group of individuals who will choose the EHR and ensure the implementation is successful. The particular members of your implementation team will depend on many things, including your budget and implementation services scope.
The right implementation team will help ensure your clinicians and front-line staff have a place at the table when working on and developing workflows. Clinicians and end users must be on board with such a significant change, otherwise, it could reduce morale, increase inefficiencies, and bring the process to a halt. As these are the primary staff required to document within the system on an ongoing basis, they should be comfortable with the process.
The subject matter experts can make essential decisions regarding system workflows. These subject matter experts should know the intake-to-discharge process that you go through for all services and each level of care. They need to be able to tell the implementation team why they do things a certain way. (If they can’t, it may mean you need to update that process.)
Understand workflow & documentation requirements before implementation
You must understand your organization’s current work process to know exactly how the EHR will fit within it. You may find that some changes are necessary to operate more efficiently. Will your new EHR be flexible enough to handle your current and future service lines?
Gather input from team members, surveys, and other technologies your providers use. Look for opportunities for improvement, and work with the implementation team to create a plan to address them. Be aware that an EHR may not automatically resolve preexisting inefficiencies.
Having an established, efficient workflow can also decrease the stress of EHR implementation. Make sure that each step in a workflow adds value for the client or increases staff efficiency. Finally, be sure you have enough staff members trained and ready to use the EHR. Examples of core clinical documentation include:
- Pre-Admission
- Admission
- Client Profile
- Consents to Treat & Medication
- Financials / Ability to Pay
- Authorizations
- Privacy Practices / HIPAA
- Advance Directives
- Physical & Family Histories
- Intake Assessments
- Ongoing Assessments
- Progress Notes / Care Plans
- Client Signature Tracking
- Discharge Forms
Deeply understand your payer & payer requirements
Your implementation team should review the documents and standards for specialized programs. Users should understand documentation, billable CPT codes, and all other parameters. Your EHR users should be able to correct errors and append notes. Make sure this knowledge extends to staff credentialing and organizational licensing. The EHR should support your growth into new locations, states, or services.
The software should also be able to accommodate unique programs that may not follow the “normal rules.” For example, you may receive a grant to support your specialized program. Your facility needs specific documentation to report your compliance with the grant. Examples of core service segmentation include:
- DSM V Codes
- ICD 10 Codes
- CPT Codes
- Internal Codes
- Service Description
- Service Unit
- Fee schedules
- Place of Service
- Pre-cert required?
- Referral needed?
- Licensure required?
- Modifiers required?
- Submission type?
Some of these steps may sound like micromanagement, but they don’t have to be. Think of them more like delegation—they help different tools, and people, do what they do best. Sometimes this calls for leaders to be closely involved, but other times they should sit back and let the tools do their thing.
This can help give you a perspective that may allow you to make better decisions—including how you use your EHR or even to change EHRs—based on accurate data, actual abilities, and real needs. Remember, giving everyone enough time with the EHR before deciding if it does or doesn’t work is essential.
Do you have questions about how to implement a new EHR into your organization? Let’s connect to discuss how Evolve Partners Consulting can support you during this process.


